
An inside look at the lab developing a Lyme disease vaccine for people
From tick room to treatment, VCU School of Medicine’s Richard Marconi and his lab are unlocking answers to a growing health problem.
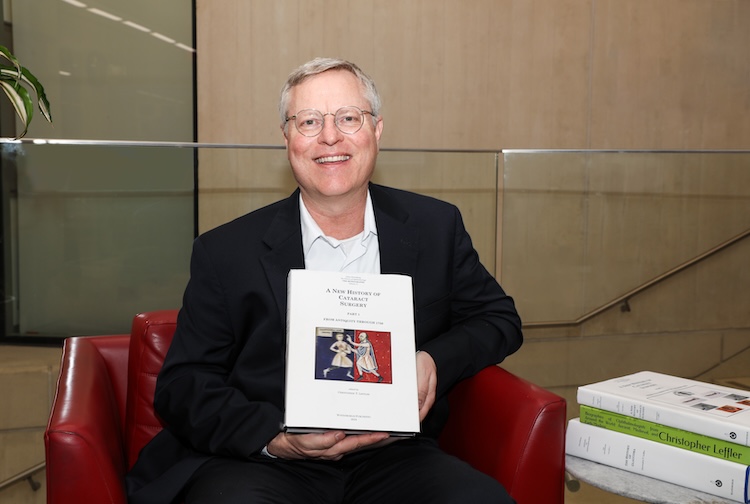
July 22, 2024 Richard T. Marconi, Ph.D., in his lab on the MCV Campus at VCU. (Daniel Sangjib Min, MCV Foundation)
Richard T. Marconi, Ph.D., in his lab on the MCV Campus at VCU. (Daniel Sangjib Min, MCV Foundation)
By Eric Peters
Tucked toward the back of a Virginia Commonwealth University School of Medicine research building, through a laboratory, around a couple of tight corners, just past pieces of equipment that accomplish tasks like “fast protein liquid chromatography,” there is a door. It’s nondescript, save for a small, lime-green, handwritten sign that reads: TICK ROOM.
Inside the broom-closet-sized room, researchers maintain live specimens of several species of ticks. Gathered from wild and domesticated animals such as deer and dogs from across the region, ticks are not hard to find — they are abundant in Virginia and can be found in any part of the state and across significant swaths of North America and Europe.
These parasitic arachnids are the reason scientists here in the lab of Richard Marconi, Ph.D., have been working for more than 30 years. They’ve been exploring and developing solutions to counteract the growing negative health outcomes related to the continent’s steady increase in tick population.
The problem is, ticks can carry and transmit several debilitating diseases, including Lyme disease, which is a serious and difficult-to-diagnose illness that affects nearly half a million Americans every year. It is transmitted through the bite of an infected black-legged tick, and it is the most common vector-borne disease in the United States. Early symptoms include a characteristic “bull’s-eye” skin rash, fever, headache and fatigue. Early detection is difficult because these symptoms can easily be taken for any number of illnesses that general practitioners are more familiar with diagnosing.
And if left undiagnosed, long-term infection can be debilitating. It can affect the joints, the heart and the nervous system, resulting in severe fatigue, arthritis, facial palsy, muscle and joint pain, numbness, carditis, heart palpitations, dizziness, shortness of breath, memory loss, cognitive impairment, depression, anxiety, insomnia, psychosis and many other life-altering challenges.
In the U.S., the number of Lyme disease cases has doubled since 2000, and it is a serious concern across the rest of the continent and in Europe.
Facing the growing threat head-on, and with decades of experience, is Marconi’s lab. There is no group anywhere in the world working harder or more effectively at the leading edge of the fight to detect and prevent Lyme disease.
In 2016, a novel, highly effective vaccine called Vanguard crLyme (Zoetis) that the team developed for dogs went to market. CrLyme is now the most widely used canine Lyme disease vaccine in North America. “The canine vaccine has taken the veterinary market by storm,” said Magdalena Morgan, Ph.D., director of licensing at VCU Tech Transfer and Ventures. It’s considered the best of several such vaccines available, thanks to its capability to fight different strains of the disease.
Nick Cramer, a Ph.D. candidate at the VCU School of Medicine, examines a black-legged tick under a microscope in the lab of Richard T. Marconi, Ph.D. Cramer is working on a vaccine and diagnostic test for ehrlichiosis, a tick-transmitted bacterial disease. (Daniel Sangjib Min, MCV Foundation)
Marconi’s team also developed a much-needed diagnostic for humans. This is hugely important because finding a diagnosis means finding the right care and, hopefully, some relief from symptoms. Just one example is Richmonder Craig Suro who, after searching for the cause of his unbearable and debilitating anxiety for six months, finally was given a Lyme disease diagnosis thanks to Marconi’s lab.
“When you hear the results, you literally stop what you’re doing and just bawl,” said Suro in 2017. “Not having a diagnosis is such torture. I don’t think Marconi has any idea what he did for me.”
To date, the Marconi Lab has enjoyed success and improved countless lives through its work, but they are not yet finished. The team now has its sights set on stopping Lyme disease in humans before it ever begins, and their initial research in developing a human vaccine has yielded eye-catching results: 100% effectiveness in a controlled lab environment.
An epiphany in the lab leads to a new approach
Marconi is a professor in the Department of Microbiology and Immunology at the VCU School of Medicine. His busy lab employs 14 people today, but when he arrived at VCU in 1994 as a 34-year-old assistant professor interested in the basic science of Lyme disease, he had to build his team from scratch.
In those early days, creating vaccines based on research — which would be called translational science — was not in the plans. Basic science and understanding were the focus.
“For the first 12 or 13 years I was here, we were studying what I refer to as the molecular pathogenesis of Lyme disease,” Marconi said. “Our initial goals were to determine how the Lyme disease spirochetes persist in the body and cause disease. What are the proteins that are involved? How do the bacteria cause damage during infection?”
Lyme disease is caused by a bacterium named Borreliella burgdorferi, which belongs to a unique group of bacteria called spirochetes, and as the name implies, they have a spiral-corkscrew-like structure. The Lyme spirochetes can produce large numbers of outer surface proteins, which interface directly with the host immune system. The Lyme spirochetes switch the proteins they make as a means of adapting to different environments and protecting themselves.
By 2007, Marconi’s team was very interested in one of these outer surface proteins — OspC. This protein is required for the bacteria to move from a tick to a mammal and cause an infection. Therefore, it is a perfect target for vaccines.
The challenge, however, in developing an OspC-based vaccine is that 30 distinct OspC variants have been identified worldwide, and any given strain of a Lyme disease bacteria only makes one version of it. Thus, using just one OspC in a vaccine wouldn’t protect against all Lyme disease strains that are producing different OspC variants.
So the Marconi Lab began to ask, “How do we make one vaccine that works against all these different variants?”
Contemplating this challenge one day in his office, Marconi and his team had an epiphany of sorts. There might be a way, they surmised, to create a brand-new single protein to be used in a vaccine that includes segments of all the most important OspC variants.
And from that day on, the Marconi Lab became a translational science lab.
The team identified the piece of OspC, known as an epitope, that triggers the immune response and found that was the part that varies so widely worldwide. Based on the earlier epiphany in Marconi’s lab, the team then invented a next-generation process they call chimeritope technology. Using this approach, they designed a DNA molecule comprising the epitope encoding sequences from several different variants of OspC. The word chimeritope is formed from the words chimeric — joining together parts of different organisms — and epitope.
Jade Smith, a Ph.D, student in the Marconi Lab, looks at a cluster of Borreliella burgdorferi cells, the bacteria that cause Lyme disease. (Daniel Sangjib Min, MCV Foundation)
“That was really the big breakthrough,” Marconi said. “It wasn’t a concept that was being pursued at the time. We were really at the lead of developing the concept of chimeritope proteins, but now it’s widely used. It’s really attracted a lot of attention.”
It had been shown decades prior that the OspC protein is a potentially good vaccine candidate. But the problem was it didn’t provide broad protection because of all the variants.
“For example, what everyone learned from COVID was that new strains can emerge and you need a new vaccine to address the new strains,” Marconi said. “It’s a little different with Lyme because new strains are not emerging, but there are many different strains that are stably maintained in nature — you need to make sure that you make a vaccine that can protect against all those different strains. The chimeritope approach is well-suited for achieving this goal.”
While it wasn’t what Marconi set out to do when he arrived in 1994, his basic benchside research built and accumulated over many years and directly led to vaccines, diagnostics and other health care tools. This is the definition of translational science: from the bench to the bedside. Or in this case, from the tick room to treatment.
An important piece of the foundation and the developments that follow, Marconi says, is philanthropic support. Private funding can quickly be put to use, and it provides resources to attract and retain skilled personnel, equipment and other tools. It also allows scientists to pursue new, unproven ideas. It enables them to explore — to be scientists. Oftentimes, donors provide seed funding for proof-of-concept studies that lead to larger funding from organizations like the National Institutes of Health.
“The importance of philanthropy can’t be understated,” Marconi said. “Without it we would not have been able to make the key breakthroughs that have led to products that benefit patients.”
A human vaccine and new diagnostic test for Lyme
The lack of a human vaccine for Lyme disease has long plagued Marconi.
“What has consistently bothered me is the notion that the best we can do in terms of prevention after so many years of study is to tuck your pants into your socks, perform ‘tick checks’ and apply sprays containing permethrin,” Marconi said. “With the increasing incidence of Lyme disease, I couldn’t accept that this was the best we could do — I thought there’s got to be a better way.”
Building on his previous basic science work and its applications in the canine vaccine crLyme — and leveraging a $2.5 million grant from the National Institutes of Health in 2019 — Marconi and his team are close to solving the human vaccine puzzle.
They’ve developed a completely new Lyme disease vaccine that uses the same chimeritope technology as crLyme, but this time uses the OspC variants that affect humans rather than the variants that affect dogs.
This past December, the team received word that the new vaccine formulation for humans yielded 100% efficacy in an elevated animal model.
“That’s really exciting, particularly when you consider that the study closely mimics the way you or I might get Lyme disease in nature,” Marconi said. “That’s the optimal way to do a challenge study, and it provided complete protection.”
Like the canine vaccine, the new human formulation incorporates an additional protein beyond the OspC chimeritope. Whereas OspC is active when the Lyme disease bacteria is inside a mammal, the OspA protein is active when the bacteria is still inside a tick. Thus, incorporating a chimeritope into the vaccine that is based on the OspA and two additional proteins that are primarily produced in ticks enables a vaccinated mammal’s blood — full of antibodies activated by the vaccine — to go into the feeding tick and target the bacteria before it ever enters the mammal. This is known as a transmission-blocking vaccine.
Transmission-blocking vaccines aren’t always effective, and focusing solely on this approach explains, in part, why previous Lyme disease vaccines have failed. When used together, however, the OspA and OspC chimeritopes developed in Marconi’s lab provide a multilevel shield against the bacteria — inside the tick and then inside the human or other mammal.
Now that the multilevel shield specially formulated for humans is in place and has shown promising results, the next steps in the process are to optimize the dosage of the vaccine and identify the perfect ratio of the two chimeritopes to elicit the optimal immune response.
As the team finalizes the human vaccine, they are also developing a new diagnostic test.
“Our strategy in the lab is that when we work on a vaccine, we simultaneously work on a diagnostic assay,” Marconi said. “That’s important because you want to make sure there is a diagnostic available that does not yield a false positive in someone who has been vaccinated.”
The exciting development in this new diagnostic is that it is being designed to work as a lateral flow test. Examples of this type of test include pregnancy, drug or COVID-19 tests in which a sample is applied to a matrix and in a short time results can be seen on an indicator.
“That’s a really nice kind of diagnostic test because it can be used by a clinician or a veterinarian in the office while that patient is there,” Marconi said. Confirmation of results can then be obtained by diagnostic laboratories.
These diagnostic and vaccine developments are moving quickly, and Marconi expects clinical trials to begin within a few years. If he keeps up the current pace and optimism in being able to battle or prevent Lyme disease, that small TICK ROOM at the back of his lab might one day better serve as an actual broom closet.




.ashx)